Here’s What You Need To Know About Bone Density
An individual’s ability to do anything diminishes significantly as they age. As we become older, our bodies undergo various physical and physiological changes. Those over the age of 65 are more likely to notice these changes. Many techniques exist for assessing bone and muscle mass loss, but DEXA scan NJ is often the most accurate and reliable.
The number of people above 65 has been steadily rising throughout time. Untreated sarcopenia and bone mass loss (osteoporosis or osteopenia) in the elderly can lead to diminished independence in old age, a major public health issue. Untreated osteoporosis or sarcopenia may raise the chance of a fall or fracture, rendering older people more vulnerable to mobility limits or severe disability that eventually limits their ability for independence. In this blog, we will discuss the burning question of whether the elderly can increase their bone density and some of the methods to do so.
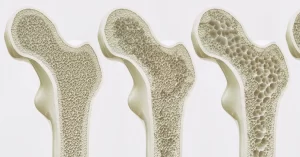
Loss in Bone Density
Osteopenia is a term used to describe the progressive decrease in bone mass. An increasing bone loss and decreased bone density are the signs of osteoporosis, a disorder that commonly develops from osteopenia. Osteopenia and osteoporosis, as well as the resulting bone fragility, are more common in older people.

Bone mass loss is caused by various factors, such as muscle mass loss. Osteoporosis is the most frequent ailment of old age. After menopause, women’s skeletons age quicker than men’s because of hormonal changes. Studies have suggested that diet, genetics, lifestyle, and comorbidities all have a role in bone density loss. There is a rapid loss of bone tissue in the latter years of life, which may be due to hereditary factors. Though the loss is irreversible, you can adapt to certain life changes that can slow down the process or help ease the painful symptoms.
Below are some of how older people can improve their bone density.
Be aware of your condition
Were you unsure about your bone-strength level? Take a few diagnostic tests like FREX and DEXA bone scans at your doctor’s office. These scans use an online application to examine your lifestyle, genetic history, health, and risk factors to predict your likelihood of developing osteoporosis in the following 10 years.
Get a bone density scan, also known as a DEXA scan, for the most accurate results. DEXA bone density test is quick, painless, and rapid. Bone mineral density is measured using low-dose X-rays on the hips and spine, lying on a cushioned cushion for the easy, noninvasive procedure. Finally, a “T score,” which measures bone density compared to women in their 30s, is calculated. Bone mineral density is considered normal if the T score is +1.0 and -1.
A score of -1 to -2.5 indicates osteopenia. Osteoporosis may be a symptom of this condition, and osteoporosis is present when the value is less than or equal to -2.5.
Take these bone density tests near me into account and then take the necessary steps afterward.
Nutrition

The loss of muscle mass and strength may be detrimental to the elderly if their diets are drastically reduced. Lower energy consumption results in weight loss and muscle mass loss due to a reduction in energy intake. From providing nutritional assistance to supplementing with particular nutrients, a variety of therapies have been examined through bone density tests. Vitamin D, protein, and various antioxidants and minerals, such as selenium, carotenoids, and vitamins C and E, have been repeatedly associated with sarcopenia and frailty in the aged.
Proteins

Proteins are important for the elderly because of their increased need for muscle mass. It is essential for muscle protein formation since ingested amino acids stimulate muscle protein synthesis. When protein is consumed with carbs, the body’s synthetic reaction to amino acid intake is lessened in the elderly. A gradual increase in protein consumption is recommended for the elderly to maintain nitrogen balance and prevent muscle loss. Sarcopenia may be slowed by taking protein along with amino acid supplements.
Strength Training

Strength training may effectively fight muscle loss by improving muscular strength and encouraging hypertrophy. As per research, older persons’ maximal lean body mass rose by 1.0 ± 0.5 kg following six months of strength training three times weekly. In a randomized controlled experiment, they tested the benefits of strength training on 91 frail elderly community members (78 and older). Thigh and body fat-free mass increased in older males and females after three months of monitored strength training. Foraged men, the research found that strength training was more effective than other forms of exercise in maintaining muscle mass and performance.
Hip Protector

Adults are more prone to breaking their hip as a result of a fall. These customized undergarments protect the hip region against a sideways fall by cushioning the area around it. The efficacy of these products has been the subject of several types of research, all of which have produced inconsistent findings. Poor patient compliance is a major downside of these devices since patients find them cosmetically unappealing and uncomfortable. Hip protectors don’t seem to be beneficial when it comes to seniors who live in the community. In addition, a major, multicenter, randomized controlled study of nursing home residents found no change in the risk of hip fracture. As a result of these findings, wearing a hip protector is not suggested as a primary method of preventing hip fractures; however, it can be used as a preventive measure.
Reduction in the consumption of tobacco and alcohol

If one has to state the factor that affects your musculoskeletal health the most, it would be excessive alcohol and tobacco consumption, as both are extremely detrimental to the bone’s health. On average, more than three drinks each day for men and two for women are likely to increase falling chances, and the same stands true for tobacco-containing products. Complications related to orthopedic perioperative smoking include a high chance of infection, impaired hearing, impaired or delayed fracture arthrodesis, and union and bad arthroplasty results.
Medications

When it comes to prescribing osteoporosis medication, many nations have different standards in place. Osteoporosis medications were shown to reduce fracture risk while also being cost-effective. As a result, treatment recommendations were developed. Any woman who has gone through menopause is eligible for therapy.
Antiresorptive and anabolic and medicines are the two main bone mass loss therapy mechanisms. Reducing bone loss with antiresorptive medicines increases bone strength. The recombinant proteins induce positive bone growth balance and bone remodeling that the anabolic agents are made of. These include Bisphosphonates, parathyroid hormone (PTH), calcitonin, hormone replacement therapy (HRT), selective estrogen receptor modulators (SERMs), and a humanized monoclonal antibody directed against the receptor activator of the nuclear factor-kappa B ligand are the main categories of drugs used to treat osteoporosis.
Hormone Replacement Therapy

The benefits of hormone replacement treatment are documented to prevent bone loss and increase bone mass in women with postmenopausal osteoporosis. Hormone treatment reduced fractures in addition to improving bone density. For women over the age of 70 participating in the Women’s Health Initiative (WHI), active treatment substantially decreased fractures; but, the WHI trial group comprised women over the age of 70 participating in the CEE medroxyprogesterone (MPA) arm. Osteoporosis prevention, alleviation of vasomotor indications, and vulvovaginal atrophy linked with menopause have all been authorized by the FDA for this kind of treatment. There is a 34% reduction in the risk of clinical vertebral fractures and hip fractures and a 23% reduction in the risk of other osteoporotic fractures after five years of hormone replacement therapy.
Testosterone

Testosterone levels decline with age in the elderly. Hypogonadal males have lower fat-free mass, knee extension force. And appendicular skeletal muscle mass than healthy controls because their testosterone levels are lower. Males over the age of 60 are at a higher risk of hypogonadism than men under the age of 80, with the latter group at risk at up to 50%. For 12 months, Doctors administered 80 mg of oral testosterone every 12 hours to 69 hypogonadal patients in a controlled, double-blinded, randomized clinical study. The results showed that lean body mass grew by 2% while fat mass dropped. The effects of testosterone on muscle are influenced by various variables, including diet, genetics, and any exercise regime. However, it is very essential to have a DEXA bone density test before selecting a particular course of action.
Estrogen

The loss of muscle mass may be linked to the decline in estrogen levels after menopause. Estrogen levels are positively correlated with lean body mass. Muscle cells possess beta estrogen receptors, which means estrogen may directly influence muscle mass. Exactly how a drop in estrogen levels affects muscle mass is yet unknown. The development of sarcopenia may be linked to increased production of pro-inflammatory cytokines such as TNF- and IL-6. Using estrogen and progestin replacement therapy of 17 best-diol and cyclic norethisterone acetate in younger women has proven to be effective in increasing lean mass and decreasing body fat mass after six months of treatment.
Exercise

Increased bone density may be achieved with weight training and walking, specifically in middle-aged and older adults. Fall prevention and muscular strengthening exercises are recommended regularly to help lower the risk of falling and fractures. By altering the micro-architectural bone arrangement, this sort of exercise has the potential to boost both bone density and strength. A 6-month Tai Chi program has been demonstrated to help reduce the frequency of falls. The danger of falling, and the fear of falling in physically inactive people aged 70 years and older and increase functional balance and physical performance. Additionally, the lowest blood sclerostin levels are seen in the most physically active persons.
Human Growth Hormone

A variety of indications for the use of human growth hormone (HGH) have been authorized by the Food and Drug Administration (FDA). HGH replacement treatment enhances muscle growth and strength in young individuals with hypopituitarism. There is a positive anabolic impact on HGH in the middle years. Thigh strength is improved in men and women over 50 with an HGH deficit that began in adulthood.
Physical Medicine and Rehabilitation (PM&R)

Physical medicine and rehabilitation have been shown to decrease disability, help improve function, and minimize the risk of recurrent falls in people with osteoporosis. However, further research is needed to confirm these findings. According to research, active living is related to a decrease in hip fracture risk of 45 percent in males. And 38 percent in women. It has been claimed that the risk of falling is typically lower among physically active persons. With a possible rise in risk among the physically inactive. Rehabilitation, in conjunction with exercise, is widely acknowledged as a technique of improving musculoskeletal function. Like the ability to perform daily life activities. Psychosocial variables have also been shown to significantly impact the functional capabilities of people with osteoporosis who’ve already previously sustained a fracture. In this case, psychological assistance and counseling may help to enhance the overall well-being and life quality of the patients involved.
Conclusion
Osteoporosis is a serious problem for the elderly. In this group, DEXA bone mineral density testing is critical and cost-effective. Current osteoporosis medicines seem to be safe and effective in the elderly. And many live a long life enough to benefit from these medications. If you are at the borderline for vitamin D toxicity, you should get it checked out by a doctor. Osteoporosis fractures are more likely to occur in the elderly; therefore, it’s crucial to consider this. Strategies to prevent fall risk are as critical as pharmaceutical treatment in this group. Osteoporosis treatment in older adults, particularly males, needs more research to comprehend the risks and advantages of pharmacological therapy.